Wolff's law states that bone will respond to the mechanical load placed on it. This can occur through modelling, which leads to a change in shape and volume of the bone to reduce stresses, or through remodelling, which involves a change to the internal structure of the bone. During remodelling, bone will be laid down by osteoblasts in areas of increased stress and resorbed by osteoclasts in areas of reduced stress. This allows for the repair of fatigued bone which has been subjected to repeated cyclical loading (Whitton et al, 2010; Markel, 2019; Logan and Nielson, 2021). Stress fractures occur during continued repetitive loading when the rate of accumulation of microdamage within the bone is greater than the ability for repair through remodelling (Whitton et al, 2018). Stress fractures can vary from subclinical microcracks to complete, catastrophic fractures.
What types of horses are affected?
Stress fractures can occur in any horse undergoing repetitive exercise, although this type of injury is most commonly diagnosed in young Thoroughbred racehorses. In a study looking at incidence of musculoskeletal injuries in a population of Thoroughbred racehorses in the UK, the tibia was the most common type of stress fracture, followed by the pelvis and the condyle of the third metacarpus (Ramzan and Palmer, 2011). Other studies have described stress fractures of the pelvis and tibia in Standardbred harness racing horses, but the reported incidence is lower than in Thoroughbred racehorses (Bertuglia et al, 2014; Puccetti et al, 2022). Stress fractures can occur at a range of locations in other performance horses – particularly event horses – however, large research studies describing these injuries in this population are limited (Hayton and Sneddon, 2004).
Diagnosis
Stress fractures should always be considered as a differential diagnosis in performance horses with a moderate to severe lameness, particularly young Thoroughbred racehorses. In many cases there are no localising signs and further diagnostics are required. Diagnostic analgesia should be used with caution in this population of horses because of the risk of fracture propagation; therefore, diagnostic imaging is frequently relied on to make a definitive diagnosis. Some stress fractures may be evident radiographically as radiolucent lines or by callus formation in more chronic cases, while others may never be detectable on radiographic examination. Nuclear scintigraphy is often the diagnostic technique of choice for early diagnosis of acute stress fractures or fatigue injuries. Magnetic resonance imaging and computed tomography can also be useful for further assessment of the injury and to guide treatment. In lower limb fractures where the exact orientation of the fracture is uncertain, standing magnetic resonance imaging and computed tomography are generally preferred, to avoid the risk of general anaesthesia and fracture propagation.
Prevention
Prevention of stress fractures and fatigue injuries usually requires modification of the training regimen. Some suggestions include a reduction in the distance of fast work, an increase in time period between races or competitions, shorter training periods and longer rest or recovery periods (Verheyen et al, 2006). However, further research is required to determine the optimal training conditions to prevent these injuries.
Condylar fractures of the third metacarpus/tarsus
Fractures of the distal third metacarpus/tarsus are one of the most common injuries in Thoroughbred racehorses in the UK, and have been associated with a high number of fatalities during National Hunt racing (Allen et al, 2017). Fractures of the distal third meta-carpus/tarsus most commonly affect the lateral condyle, although the medial condyle may also be affected (Parkin et al, 2004). These fractures generally originate in the region of the parasagittal groove and propagate proximally in a sagittal plane (Riggs, 1999; Zekas et al, 1999; Jacklin and Wright, 2012). Repetitive training leads to an increased bone density within the subchondral bone of the distal metacarpal/tarsal condyles. This is seen as a region of sclerosis on radiographs. Densification of the condyles compared to the sagittal ridge may cause a density gradient, which leads to the concentration of shear forces at the parasagittal groove (Riggs et al, 1999; Kawcak et al, 2000; Rubio-Martinez et al, 2008). Additionally, microcracks formed during cyclic loading have been shown to accumulate and coalesce, leading to subchondral bone cracks and eventual fracture propagation (Stepnik et al, 2004).
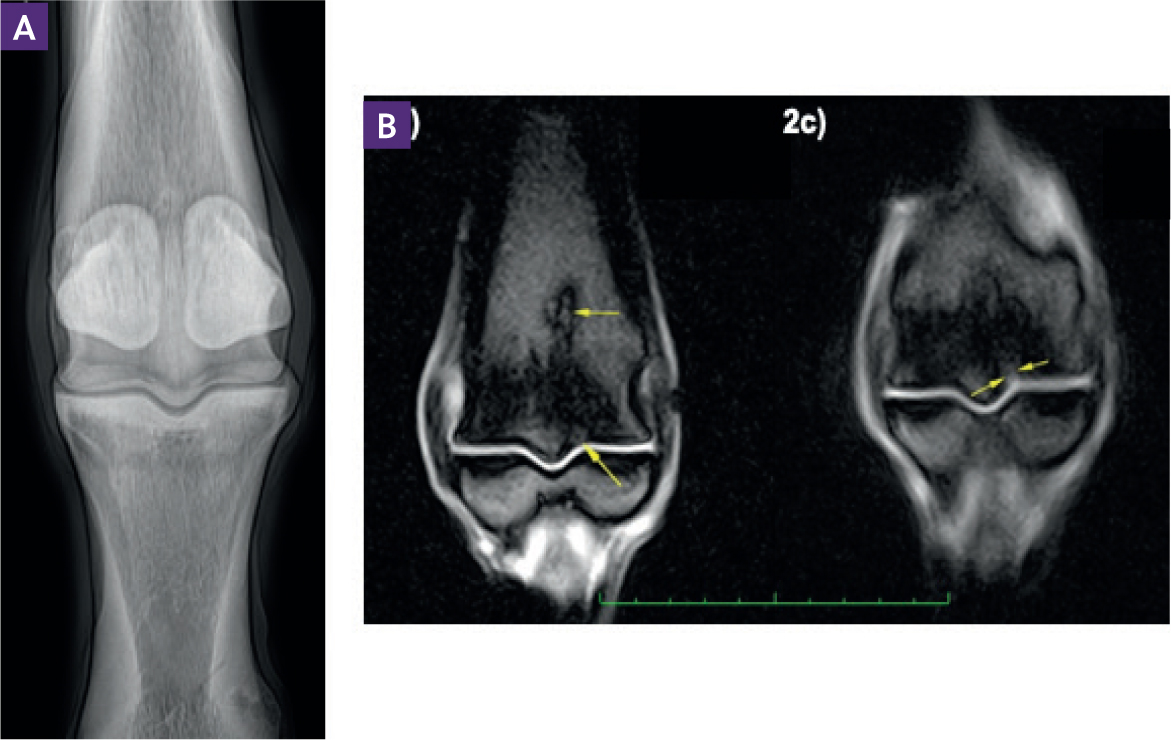
Condylar fractures can present in a variety of ways. Horses with short fissure fractures may show a mild lameness without evidence of localising signs, while horses with incomplete or complete fractures tend to show a moderate to marked lameness with evidence of fetlock joint effusion. Incomplete or complete condylar fractures can often be diagnosed based on clinical signs and radiography; good quality flexed dorsopalmar/plantar radiographic views must be included (Ramzan et al, 2015) (Figure 1). Fissure fractures may require additional imaging, such as magnetic resonance imaging, to make an accurate diagnosis (Figure 2). Nuclear scintigraphy can also be a useful technique for the diagnosis of stress-related condylar injury in the acute stages; however, differentiation between increased radiopharmaceutical uptake in the condyle and the proximal sesamoid bone can be challenging. If these fissure fractures are not detected, then they can propagate with continued training. With regard to incomplete or complete condylar fractures, those occurring laterally tend to be simple fractures that exit the cortex within the diaphysis of the bone, while medial condylar fractures are often incomplete and extend proximally with a spiral configuration (Figure 1).
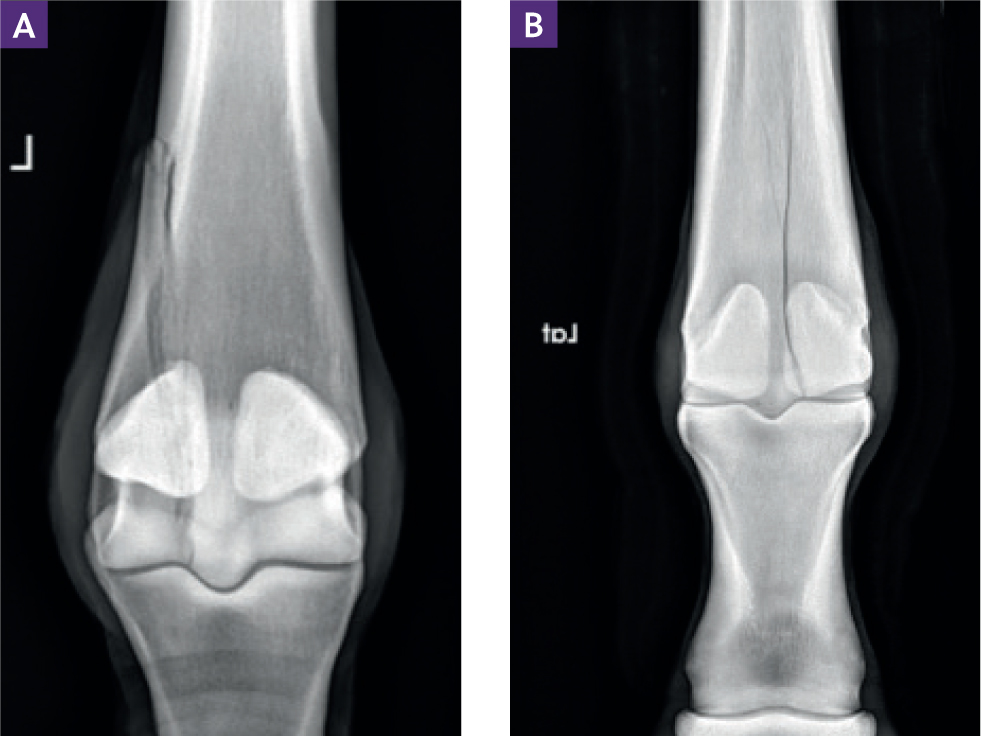
Both lateral and medial condylar fractures can occur in either the forelimb or the hindlimb. However, a medial configuration was reported more commonly in hind limbs in one case series (Martin, 2000) and and more likely to spiral in medial condylar fractures in another case series (Ellis, 1994). This spiral configuration is more likely to result in propogation and catastrophic failure. Therefore, horses with medial condylar fractures of the hind limb should be placed in cross-ties prior to surgical repair.
Internal fixation is the treatment of choice for all condylar fractures, other than extremely small fissure fractures which can be managed conservatively with box rest, followed by gradually increasing in-hand walking exercise (Payne and Compston, 2012; Wright and Nixon, 2019). In most cases, conservative management of condylar fractures should only be considered if there are financial constraints preventing internal fixation. Standing fracture fixation with cortex screws placed in lag fashion can be used to treat most non-displaced and incomplete lateral condylar fractures, thereby reducing the risk of general anaesthesia (Payne and Compston, 2012). Medial condylar fractures of the hind limb with a spiral configuration usually require plate fixation under general anaesthesia (Goodrich et al, 2014).
The prognosis for return to athletic function is good (70–80%) in horses with incomplete lateral condylar fractures and without pre-existing osteoarthritis of the fetlock joint (Rick et al, 1983; Bassage and Richardson, 1998; Zekas et al, 1999). The prognosis for return to previous level of work is around 50% in horses with displaced lateral condylar fractures and 40% in horses with medial condylar fractures following surgical management (Goodrich et al, 2014).
Palmar/plantar osteochondral disease
Palmar/plantar osteochondral disease is an injury that occurs as a result of accumulated stress during high-speed exercise in race-horses. This leads to subchondral bone microdamage and sclerosis of the load-bearing regions at the palmar/plantar aspect of the third metacarpal/tarsal bone (Kawcak et al, 2000; Barr et al, 2009). Horses with mild palmar/plantar osteochondral disease lesions may be asymptomatic, but many will present with a lameness of insidious onset or non-specific signs of poor performance. This condition often affects bilateral limbs, leading to a shuffling gait with increased discomfort on a firm surface compared to a soft surface. Lameness will often improve following a low four-point nerve block or diagnostic analgesia of the metacarpo/tarsalphalangeal joint.
Radiography has low sensitivity for the detection of these lesions, but can be useful in moderate to severe cases. The most useful radiographic projections for the diagnosis of these lesions include lateromedial and flexed lateromedial projections of the metacarpo/tarsophalangeal joint. Additionally, a flexed dorsopalmar/plantar projection can provide better visualisation of the palmar/plantar aspect of the metacarpal/tarsal condyles. Radiographic findings can include focal regions of sclerosis (Figure 3b) or radiolucencies in the palmar/plantar aspect of the third metacarpal/tarsal condyle. A post-mortem study identified a predilection for lesions in the medial condyle of the forelimb and the lateral condyle of the hind limb (Pinchbeck et al, 2013a).
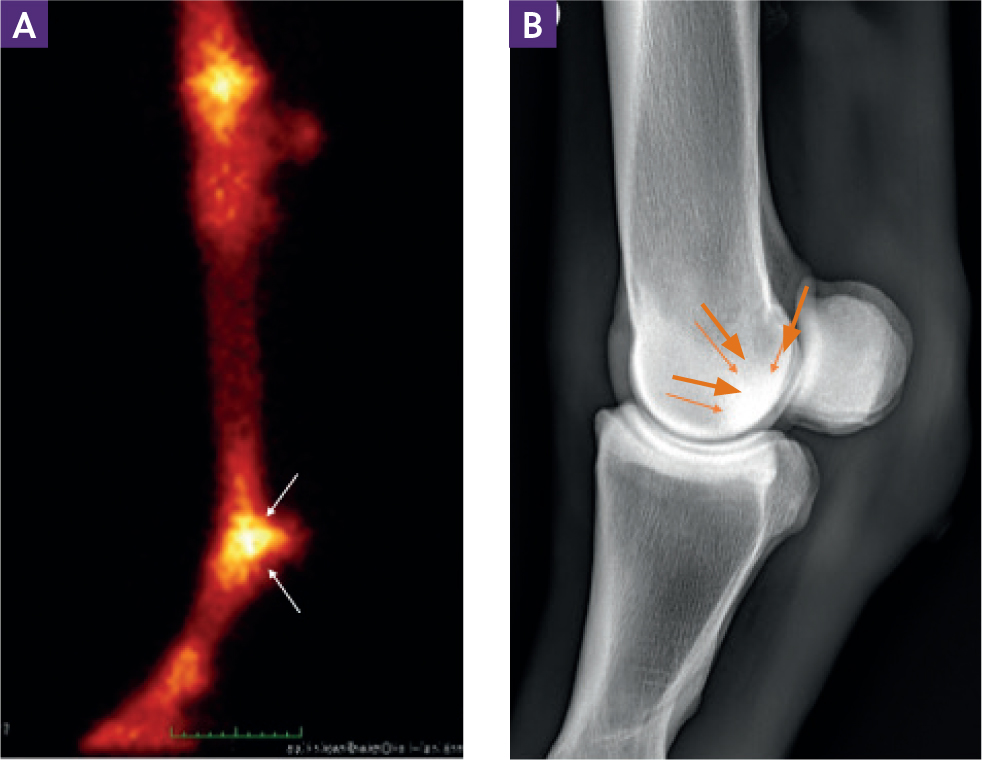
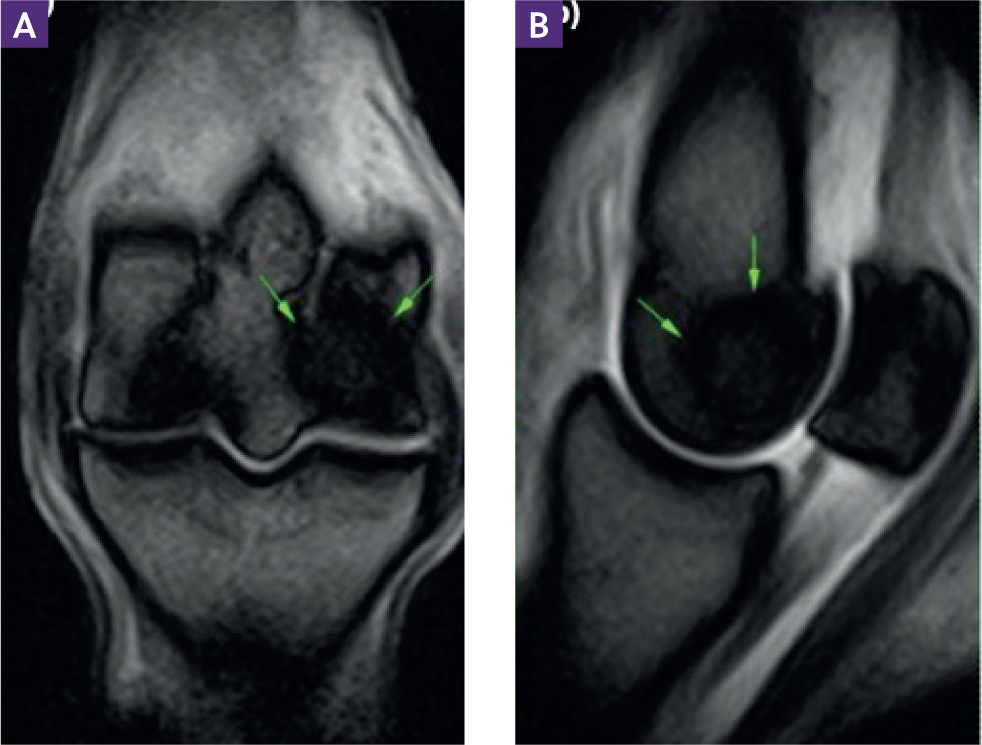
A moderate to marked increase in radiopharmaceutical uptake is often seen on nuclear scintigraphic examination of horses with palmar/plantar osteochondral disease (Figure 3a). Magnetic resonance imaging is currently the best imaging modality to detect and assess the severity of palmar/plantar osteochondral disease lesions (Figure 4). In a study of 131 racing Thoroughbred horses with metcarpo/tarsophalangeal joint pain, half showed evidence of palmar/plantar osteochondral disease on low-field magnetic resonance imaging (Powell, 2012). Additionally, magnetic resonance imaging can help to differentiate between a palmar/plantar osteochondral disease lesion and an early fissure fracture.
Treatment options for this condition are limited and usually include intra-articular medication and a change to the training programme. In a study by Pinchbeck et al (2013b), increased training intensity and number of races was associated with a higher grade of palmar/plantar osteochondral disease, while a longer period between races or after the last race was associated with a lower palmar/plantar osteochondral disease grade. These findings suggest that these lesions may heal with appropriate management. Although the prognosis for racing with this disease can vary, it is not associated with an increased risk of condylar fracture formation (Barr et al, 2009).
Osseous cyst-like lesions of the proximal phalanx
The aetiopathogenesis of subchondral bone cysts is multifactorial, and several mechanisms have been suggested. Osseous cyst-like lesions that develop in adult horses are thought to be the result of trauma to the articular cartilage and/or subchondral bone or a repetitive load injury. This creates a communication between the sub-chondral bone and the joint which allows synovial fluid to enter this area, leading to pressure and necrosis of the adjacent bone (Jackson and Fürst, 2019).
Osseous cyst-like lesions can cause variable degrees of lameness with either gradual or acute onset. Horses are often positive to flexion of the affected joint and the lameness usually improves following diagnostic analgesia of the joint. Radiographic findings include an oval radiolucency surrounded by a sclerotic rim. A communication with the joint may or may not be evident on plain radiography. Intra-articular contrast radiography can be helpful to determine the presence of a communication. Some osseous cyst-like lesions can be missed on radiography, so other imaging modalities such as computed tomography or magnetic resonance imaging may be required for diagnosis. Additionally, magnetic resonance imaging and computed tomography provide useful information adjunctive to radiographic studies regarding concurrent pathologies, presence of adaptive bone remodelling within the surrounding bone and soft tissue involvement. These modalities should be considered to confirm the diagnosis before treating these cases.
Conservative management of these lesions can include rest, non-steroidal anti-inflammatories, intra-articular or intralesional medication with corticosteroids. Surgical treatment can include arthroscopically-guided intralesional medication with corticosteroids, arthroscopic debridement, transcortical drilling of the lesion or screw fixation. A study using low-field magnetic resonance imaging to detect osseous trauma in the proximal aspect of the proximal phalanx found no difference between conservative management and placement of a 4.5 mm cortical screw across the lesion in lag fashion (Lipreri et al, 2018).
Humeral stress fractures
Stress-related injuries of the humerus can occur in response to repetitive loading and are commonly reported in Thoroughbred race-horses, as well as less frequently in endurance horses (O'Sullivan and Lumsden, 2003; Misheff et al, 2010). This can lead to a stress fracture or a complete, catastrophic fracture. Stress fractures of the humerus usually present with a moderate to severe forelimb lameness and have been reported to occur at three main sites within the bone: caudoproximal, craniodistal and caudodistal (O'Sullivan and Lumsden, 2003; Sammons and Stover, 2009). This injury can occur in racehorses at any stage of training; however, one case series found a greater risk of complete humeral fracture in horses following an increase in exercise after a rest period of 2 months or more (Carrier et al, 1998). Additionally, humeral stress fractures are more common in 3-year-old racehorses and those with a longer racing career (O'Sullivan and Lumsden, 2003). Caudoproximal humeral stress fractures tend to be more severe than those at other predilection sites and are most commonly associated with complete fractures (Dimock et al, 2013).
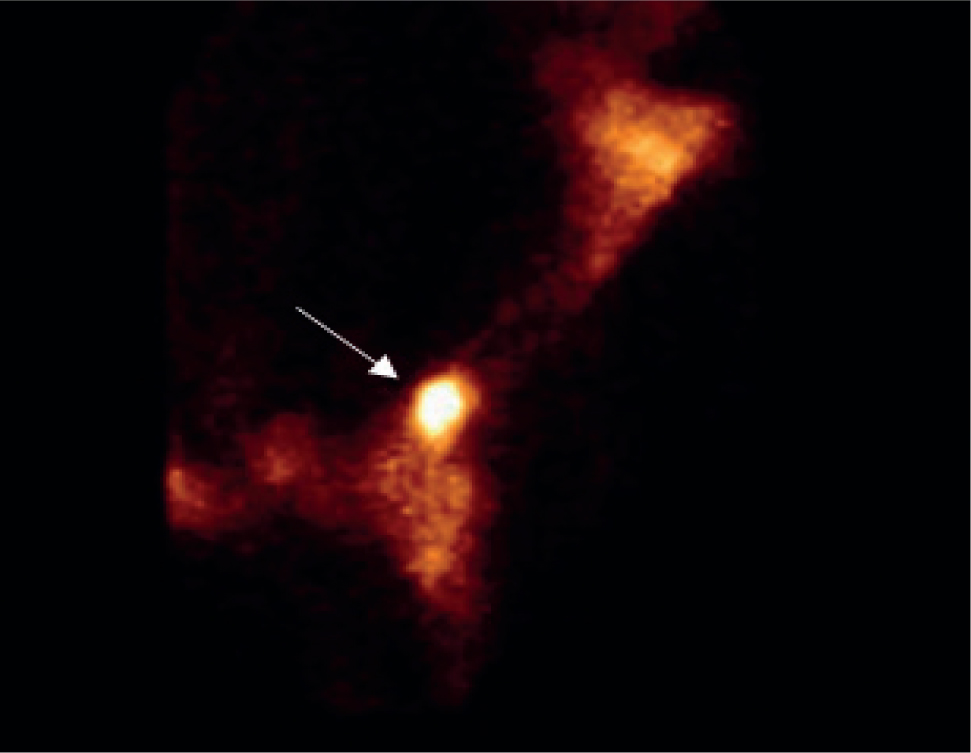
Humeral stress fractures can often be diagnosed based on clinical examination and radiography. Radiographic findings for horses with incomplete fractures include periosteal new bone formation and sclerosis. The three predilection sites should be examined carefully for these changes. If there are no localising signs, or radiographic examination shows no significant findings, then nuclear scintigraphy is recommended to allow for early diagnosis. Focal increased radiopharmaceutical uptake at one of the predilection sites within the humerus is considered conclusive for diagnosis of a humeral stress fracture (O'Sullivan and Lumsden, 2003) (Figure 5).
There are few reports of surgical repair of complete humeral fractures, suggesting that immediate euthanasia is usually warranted in these cases. Incomplete humeral stress fractures can be treated conservatively. This should include box rest for around 8 weeks with the introduction of in-hand walking once the horse is sound. The prognosis for return to racing following an incomplete stress fracture of the humerus is excellent, although one study reported a 15% fracture recurrence rate, usually involving the contralateral limb (O'Sullivan and Lumsden, 2003). These horses should be monitored carefully on return to training.
Tibial stress fractures
Tibial stress fractures are commonly diagnosed in young Thorough-bred racehorses. Repetitive training causes an accumulation of microdamage, eventually leading to an acute-onset, moderate to severe lameness. This lameness can often resolve between periods of fast exercise and then recur. A unilateral lameness is most common in these cases, although this injury can be bilateral. Three predilection sites have been identified for tibial stress fractures: the proximolateral aspect of the cortex, the caudal cortex of the mid-diaphysis and the caudal cortex of the distal third of the tibia (O'Sullivan and Lumsden, 2003). A recent post-mortem review in Thoroughbred racehorses found an association between pre-existing stress fracture and complete tibial fracture. The majority of the complete fractures in the study were associated with stress fractures in the proximolateral aspect of the tibia under the head of the fibula (Samol et al, 2021). Tibial stress fractures occur most frequently in unraced 2-year-old Thoroughbreds (O'Sullivan and Lumsden, 2003).
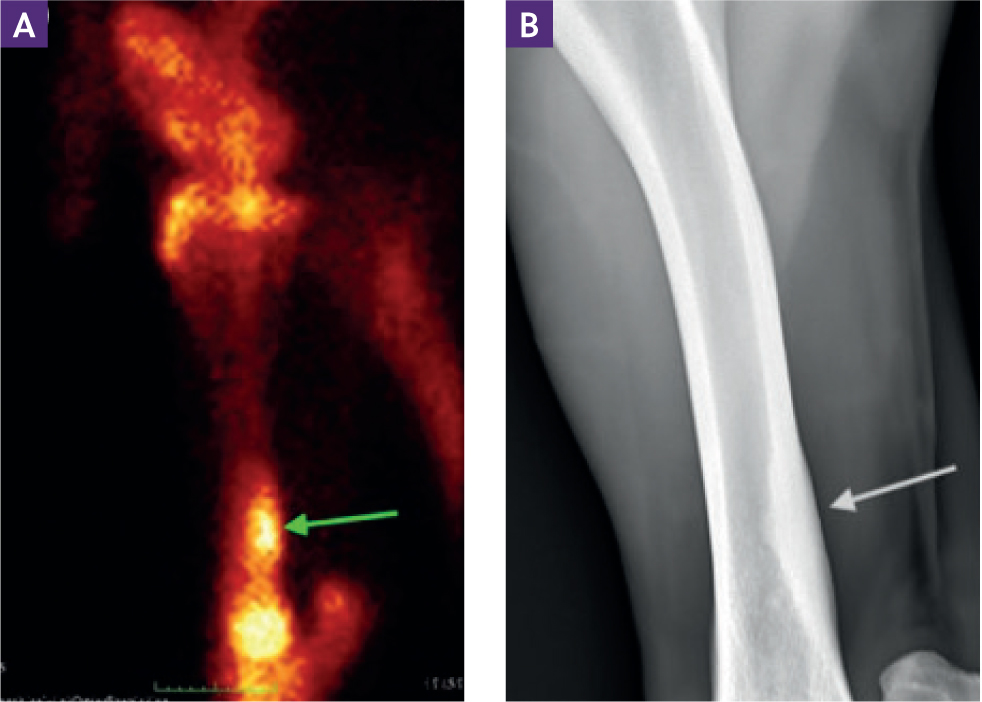
The history and clinical signs may often be suggestive of a tibial stress fracture. In some cases, palpation of the medial aspect of the tibia may elicit a pain response. Diagnostic analgesia is usually avoided in these cases, and instead diagnostic imaging is used to confirm the diagnosis. Radiographic examination is only moderately sensitive for the identification of tibial stress fractures, particularly in the acute stage. Repeat radiographic examination 7–10 days after the injury may identify endosteal and periosteal callus formation. However, the lack of significant findings does not rule out a tibial stress fracture (O'Sullivan and Lumsden, 2003). In these cases, nuclear scintigraphy is recommended, as this has better sensitivity for the identification of tibial stress fractures. Characteristic patterns of marked focal radiopharmaceutical uptake are identified at the predilection sites (Figure 6).
Treatment of incomplete tibial stress fractures usually requires a period of box rest and walking exercise. Once the horse is sound, trotting exercise may be introduced (O'Sullivan and Lumsden, 2003). These injuries usually require 6–10 weeks without exercising at canter. In cases of severe injury, where fracture propagation and displacement is considered a risk, cross-tying or slinging may be required. Complete tibial fractures in adult horses are usually considered catastrophic and require immediate euthanasia.
Tibial stress fractures generally have a good prognosis for return to racing. One study reported that 80% of 61 horses with tibial stress fractures returned to racing with no significant effect on earnings (O'Sullivan and Lumsden, 2003). Another study looking at 35 tibial stress fracture cases with a median rehabilitation time of 136 days reported a 77% rate of return to racing with no difference in race placings (McGlinchey et al, 2017).
Stress fractures of the pelvis
Stress fractures of the pelvis typically involve the ilial wing and, less commonly, the ilial shaft. These injuries can vary from subtle, incomplete fractures to severe, displaced, catastrophic fractures. Displaced fractures of the ilial shaft can lead to fatal internal bleeding, usually from the internal iliac artery. Ilial stress fractures are widely documented in Thoroughbred racehorses. One study found that 16% of fractures seen in a population of Thoroughbred flat racehorses in the UK were ilial fractures and of these, 87% were fatigue fractures (Verheyen and Wood, 2004). Fractures of the ilial wing in Thoroughbred racehorses tend to originate at the caudal aspect of the ilial wing and extend cranially over the sacroiliac joint.
Horses with pelvic fractures usually present with an acute onset hind limb lameness during or after exercise. The degree of lameness will often be associated with the severity of the fracture. Some horses may show no localising signs while others will show pain on palpation of the ilial wing, external swelling, asymmetry of the osseous landmarks of the pelvis or crepitus when flexing the limb (Rutkowski and Richardson, 1989). In horses with ilial shaft fractures, a haematoma may be palpable on rectal examination.
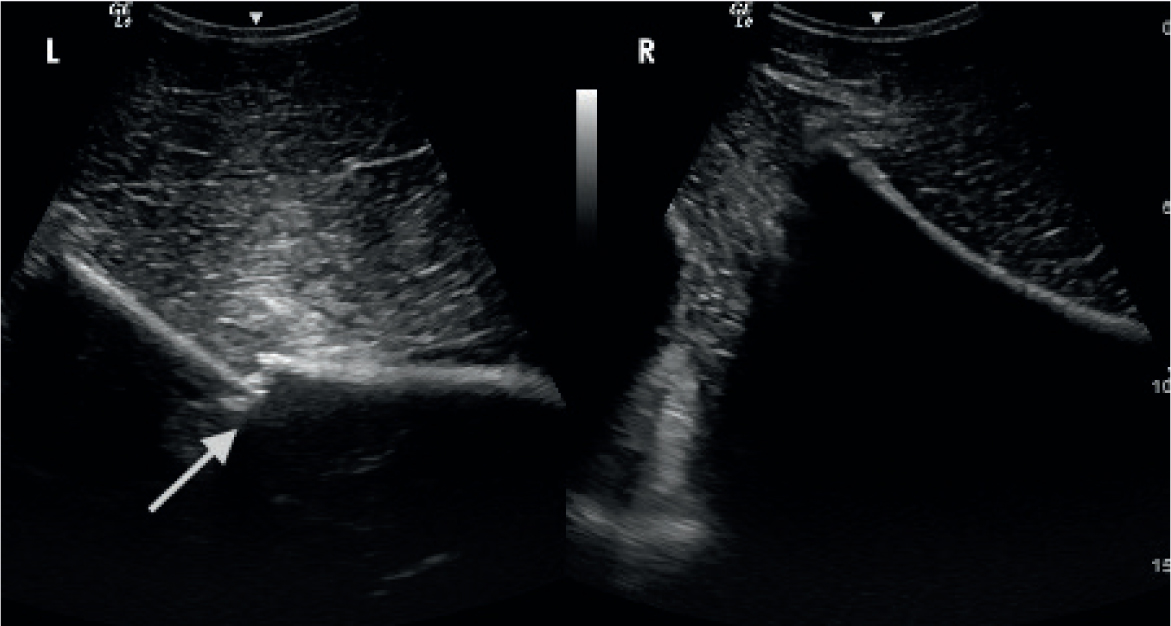
Transcutaneous ultrasound can be used to diagnose stress fractures of the ilial wing. Findings include callus formation and discontinuity in the contour of the bone (Figure 7). Ultrasound examination of the ilial shaft to diagnose an incomplete stress fracture can be more challenging (Tomlinson et al, 2001). The absence of pathology on ultrasonography does not rule out a stress fracture, so in cases with high clinical suspicion, other imaging modalities should be used. Transrectal ultrasound may be useful for diagnosing a haematoma associated with a stress or complete fracture. Nuclear scintigraphy can be used to give a more definitive diagnosis of ilial stress fracture, although the pattern of radiopharmaceutical uptake can be variable (Davenport-Goodall and Ross, 2004). Radiographic examination of the pelvis in the standing horse has been described, but this requires a high output X-ray generator and the sensitivity is low in adult horses.
The management of pelvic stress fractures must be determined by the suspected severity of injury, but is almost exclusively conservative. Horses with mild lameness and a stress fracture that could only be diagnosed on nuclear scintigraphy may be managed with box rest and a short period of walking exercise. If the lameness is moderate but the fracture is non-displaced, then 6 weeks box rest and walking exercise is usually advised. If there is a severe lameness, evidence of fracture displacement on ultrasound or a fracture of the ilial shaft, it is recommended that the horse is cross-tied for 6–10 weeks until there is evidence of callus formation on ultrasound and the horse is more comfortable. Analgesia and support of the contralateral limb is often required. Haemorrhage as a result of fracture displacement is a risk for several weeks after injury. The prognosis for displaced or non-displaced ilial wing fractures in Thoroughbred racehorses is good in horses that survive the initial period post-injury (Hennessy et al, 2013).
Conclusions
Repetitive, high-speed exercise can lead to a range of stress-related injuries in the horse. It is important to be aware of these injuries when treating performance horses to allow targeted diagnostic imaging, appropriate management and prevention of catastrophic injury. Future research may allow us to predict these injuries earlier and guide modification of training programmes.
KEY POINTS
- Stress fractures are an important differential diagnosis in performance horses with a moderate to severe lameness.
- Stress fracture or fatigue injuries can occur at a variety of anatomical locations with different clinical presentations, ranging from subclinical to catastrophic fractures.
- Diagnostic analgesia should be used with caution in a performance horse with a possible stress fracture, because of the risk of fracture propagation.
- A combination of radiography and other advanced imaging modalities is often required to give an accurate diagnosis, determine the best treatment option and guide prognosis in horses with stress fractures.


