Equine asthma syndrome (EAS) is the umbrella term used for a wide spectrum of non-septic lower airway diseases. These range from mild-to-moderate reversible equine asthma, previously termed inflammatory airway disease, to severe and potentially irreversible equine asthma, the new terminology for conditions known as heaves, chronic obstructive pulmonary disease and recurrent airway obstruction (Pirie et al, 2016). Severe EAS is differentiated from mild-to-moderate EAS by the presence of increased respiratory effort and distress at rest (Couëtil et al, 2016). Based on a questionnaire of the general equine population in the UK, the prevalence of the severe form is estimated at 14% (Hotchkiss et al, 2007). However, mild-to-moderate EAS (often subclinical) is thought to affect a much higher percentage of the population, although exact figures are unknown. Therefore, when admitting and observing horses in a hospital environment, it is likely to be one of the most common subclinical respiratory conditions encountered.
Many cases of EAS will be mild-to-moderate and may not have been noticed by the owner, given that the clinical signs are often only noted during exercise or present as an occasional cough at rest (Couëtil et al, 2016). Furthermore, cases admitted to the hospital may have well managed severe EAS, which may become exacerbated once a horse is exposed to allergens within the hospital environment. Hence, it is important to ascertain from owners on admission whether horses have had severe EAS, and monitor patients for flare-ups of clinical signs, which can include chronic coughing, raised respiratory rates, mucoid nasal discharge and respiratory distress in an afebrile horse (Mazan, 2018). Prompt discussion with colleagues and the veterinary team can guide diagnostics and reduce morbidity within the hospital environment. This is especially important given that coughing can also be attributable to highly infectious respiratory disease (Table 1).
Table 1. Common differential diagnoses of adult coughing horses within the hospital
| Infectious | Non-infectious |
|---|---|
| Equine influenza | Equine asthma syndrome (severe) |
| Equine Herpes virus (1/4) | Equine asthma syndrome (mild-to-moderate) |
| Strangles | Foreign bodies |
| Bacterial pneumonia | Left-sided heart failure |
| Aspiration pneumonia | Tracheal collapse (rare) |
| Pulmonary abscessation | Upper repiratory tract obstructions (rare) |
The clinical signs and inherent airway hypersensitivity in cases of EAS have been attributed to high levels of organic dust in the environment and magnitude of aeroallergen exposure. Environmental dust causes marked aseptic inflammation, as evidenced by an elevated neutrophil count on bronchoalveolar lavage samples (Robinson et al, 2003), which is considered the gold standard field test for diagnosing EAS (Couëtil et al, 2016). Interestingly, exposure to dust early on in life can predispose a horse to EAS, hence reduction of environmental dust is important at all ages (Hotchkiss et al, 2007). As it is difficult to identify cases of mild-to-moderate EAS before admission to hospital, it is presumed beneficial to implement practices that reduce overall dust exposure within common airspaces. This is important, because only changing stable management on an individual basis has minimal minimal impact on reducing dust within a horse's breathing zone (Clements and Pirie, 2007b).
The importance of stable dust
As stated previously, environmental organic dust exposure, predominantly from the stable environment and from sources of feed, is a major inciting cause of the immunological response associated with EAS (Ramseyer et al, 2007). When the dust is less than 5 microns in diameter, it is small enough to penetrate the lower airways and cause inflammation, which is known as respirable dust (Clements and Pirie, 2007a). Stabling and subsequent exposure to dust has long been linked to EAS, and there is increasing evidence that respirable dust is also associated with the neutrophilic inflammation in racing thoroughbreds (including those with mild subclinical EAS) (Ivester et al, 2018). This can lead to increased tracheal mucus scores (Millerick-May et al, 2013) and subsequent poor performance (Holcombe et al, 2006).
Respirable dust consists of a wide complexity of proinflammatory particles including endotoxins, fungi, moulds and ß-glucans (Samadi et al, 2009). The exact significance of each one in inciting EAS is currently unknown, although moulds and endotoxins appear to play a major role in pathogenesis (Pirie et al, 2003a). Minimising exposure to respirable dust appears to be the best way to prevent EAS recurrence, compared to pharmacological treatment (Couëtil et al, 2005).
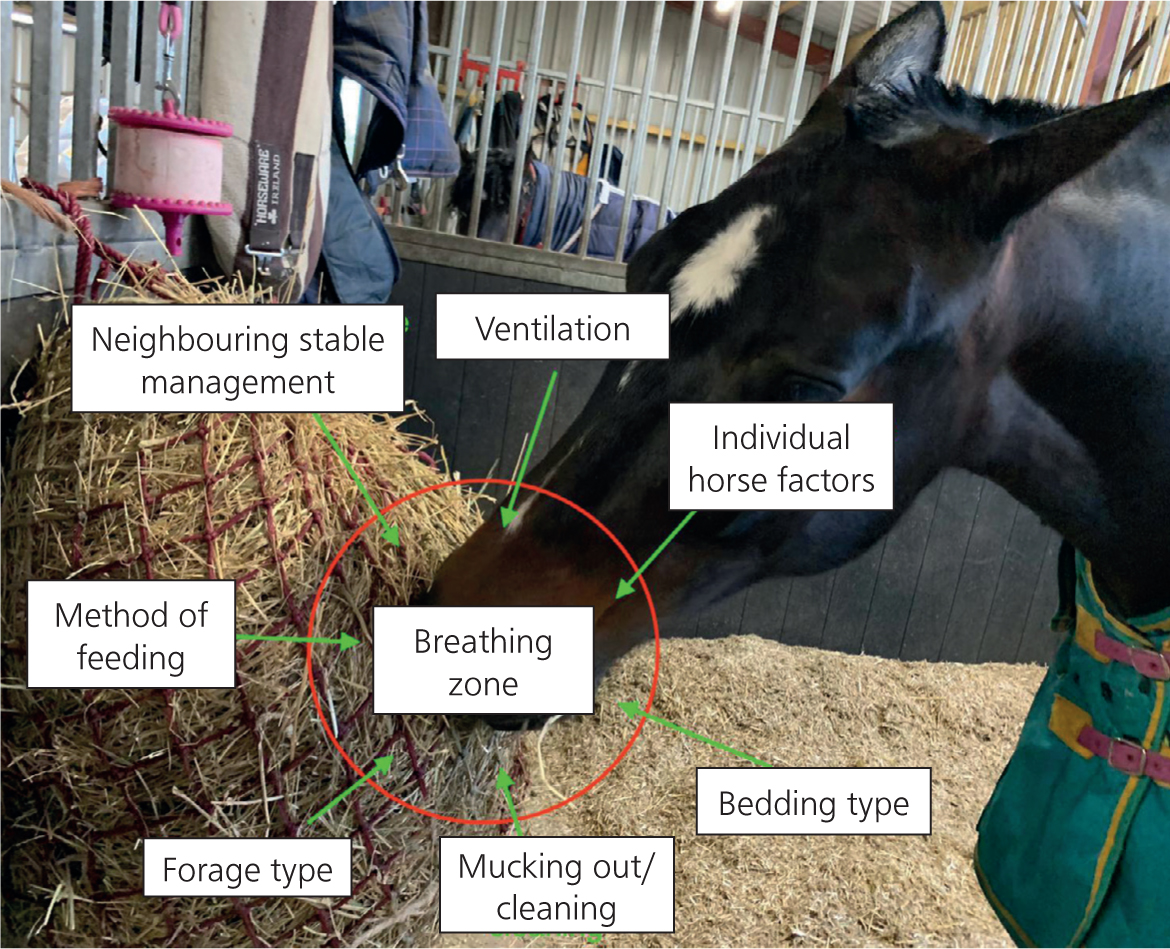
The breathing zone
Before understanding how to reduce respirable particle exposure, it is essential to understand the concept of a horse's breathing zone (Figure 1). This effectively is the area within 30 cm of a horse's nose and provides the most accurate representation of a horse's respirable particle exposure (Woods et al, 1993). Normally, the innate defence of the horse's respiratory system is able to prevent respirable dust from reaching the lower airway. However, at times of high challenge, this defence is overwhelmed. This concept is most evident when considering the method of feeding and forage type, since quadruple the exposure to respirable particles within the breathing zone is found in horses fed with hay nets, compared to feeding from the floor (Ivester et al, 2012). Horses with EAS should therefore always be fed from the floor unless other factors warrant feeding from a hay net. Increased dust exposure is thought to be a result of respirable particles being pulled into the horse's breathing zone during the tearing of the hay from the hay net (Mazan, 2018). Objective analysis of dust exposure within the breathing zone is becoming more widely available (for example, using systems such as the DustTrak areosol monitor), although no respirable response thresholds are currently confirmed. However, it may be useful to monitor alterations in the management of these horses and their impact on respirable particle exposure.
What to feed and how
Given the time horses spend grazing each day, forage is regularly in the horse's breathing zone and therefore plays the greatest role in causing EAS (Clements and Pirie, 2007). Hay, especially if bailed when wet, may be rich in fungal spores (Séguin et al, 2012) and endotoxins, which have been positively correlated with the severity of clinical signs in cases of severe EAS (Pirie et al, 2003b). Interestingly, a reverse correlation has been identified between lower airway inflammation and endotoxins in low dust environments in racing Thoroughbreds (Ivester et al, 2018). While the reason for this is currently unknown, dust exposure appears to play differing roles in mild-to-moderate EAS, compared with severe EAS. However, fungal spores play a major role in the induction of neutrophilic inflammation in both normal and susceptible horses (Beeler-Marfisi et al, 2010). Therefore, irrespective of which method is used to reduce respirable dust concentration in hay, a low mould concentration is useful for preventing the exacerbation of EAS (Earing et al, 2013). The testing of each batch of hay by an accredited laboratory, both within a hospital environment and at home, for mould content should thus be recommended.
Obviously, removing forage and feeding a completely dust-free pelleted diet will be preferable for reducing disease exacerbation, but this is rarely practical or economical in commercial practice. One alternative method of significantly reducing respirable particle concentration is soaking hay for at least 30 minutes, which reduces its respirable particle content by up to 60% (Blackman and Moore-Colyer, 1998; Clements and Pirie, 2007b; Hotchkiss et al, 2007). Simply sprinkling the hay with water is not effective. To help with the process, commercial hay soakers are available, or hay can be placed in bins with appropriate drainage for the allotted time. The same can be done for complimentary feed, where wet/cleaned and steamed mixes should be considered in preference to feeding rolled grains such as oats and barley (Hessel et al, 2009). This is especially important if feeding supplementary feed taken from the bottom of food bins, where mould and endotoxin concentrations may be at their highest. In horses with a history of severe EAS, this practice should be avoided altogether.
Time spent soaking the hay is important, as periods greater than 2 hours can significantly reduce nutrient content (Blackman and Moore-Colyer, 1998) and water-soluble carbohydrate concentration (Longland et al, 2011). Furthermore, soaking hay at very high temperatures (>15°C) can increase bacterial load (Moore-Colyer et al, 2014) and cause changes in the microbiome linked to colic (Curtis et al, 2019), although this effect is more likely to be non-linear the higher the temperature reached. Care must therefore be paid to ensure conditions are appropriate for correct hay soaking, and owners should be given advice at discharge to ensure compliance, especially since adherence to these changes is typically poor (Hotchkiss et al, 2007; Simões et al, 2020). However, in obese horses or in those requiring reduced nutrient content, it can be a useful, cheap and quick way of reducing EAS incidence.
Alternatively, hay can be steamed, if practical and with the help of commercial steamers, as this greatly reduces respirable particles and mould by up to 90% without affecting nutrient content or palatability (Moore-Colyer et al, 2016). When steamed correctly, horses fed this substrate have a lower incidence of mild-to-moderate EAS (Dauvillier et al, 2019). However, inappropriate steaming (for example, with kettles or in bins) is less beneficial and does not properly alter microbial and subsequent endotoxin content (Moore-Colyer et al, 2016). Despite this, if used appropriately, steaming appears a safe way to feed all horses prone to EAS in a hospital environment, where added nutritional value is needed.
If horses are not obese or showing signs of an underlying metabolic disease, the feeding of haylage can be an option. If cut and bailed effectively in an airtight environment, haylage contains less respirable particles than hay, owing to its higher moisture content (Séguin et al, 2012; Siegers et al, 2018). The feeding of haylage is associated with a 60–70% lower respirable particle concentration compared to dry hay (Clements and Pirie, 2007a), which is comparable to appropriate soaking of hay. It is also easier, less labour intensive and less expensive than soaking or steaming hay to reduce dust exposure. However, it is important to select appropriate patients because of the high sugar content being associated with increased incidences of hyperinsulinaemia and hyperglycaemia compared to other forages (Carslake et al, 2018). Nonetheless, it appears to be an excellent forage to use in the management of appropriately selected EAS patients.
What to bed down on
Choice of bedding is important because of the impact it has on the horse's breathing zone when the horse disturbs it, eats from the floor or is sleeping. Straw (considered to be the worst choice) and sawdust bedding are associated with severe EAS (Simões et al, 2020) because of the higher respirable particulates found in these bedding substrates (Vandenput et al, 1998). Therefore, despite their economic benefits, horses should ideally not be bedded down on straw or sawdust in the hospital. Swapping to cardboard bedding can reduce mould and respirable dust particles within the stable environment by over 50% (Kirschvink et al, 2002) and should be recommended where disposal practices make it possible. Other alternatives include paper (Tanner et al, 1998) or dust-extracted wood shavings (McGorum et al, 1998; Seedorf et al, 2007). Regardless of the bedding of choice, it should be kept dry to minimise the likelihood of mould growth. The addition of rubber mats may further aid this process, as well as reducing the total amount of bedding needed within the stable. At times of hot and dry weather and subsequently increased dust exposure (Ivester et al, 2012; Auger and Moore-Colyer, 2017), light spraying of the bedding twice daily with water may help to reduce respirable particle concentration and prevent EAS exacerbation.
Managing the stable and its environment
It has long been known that, in classical non-pasture associated EAS, complete movement away from the stable to pasture can cause remission of clinical signs (Thomson and McPherson, 1984; Vandenput et al, 1998; Clements and Pirie, 2007a). Furthermore, respirable particle and endotoxin concentration is significantly less when out in pasture, compared to stabling in a low dust-environment without feeding hay (McGorum et al, 1998; Berndt et al, 2010). However, in the hospital environment this is not practical, so care must be paid to improving ventilation within the stable. Fortunately, immunological lower airway stimulation in summer pasture-associated EAS is attributed to high heat and pollen counts found in the air, usually from May to September (Bullone et al, 2016). Therefore, stabling during this time will be beneficial for these patients. As respirable particle concentration is higher in the summer (Ivester et al, 2012; Auger and Moore-Colyer, 2017), careful attention will need to be paid to ventilation during these times.
For nurses, stable design is often beyond their control. Although, interestingly, American barn systems do not provide any added benefit over traditional stables when it comes to dust exposure (Auger and Moore-Colyer, 2017). However, subjectively assessed, poorly ventilated stables appear to have a higher respirable particle concentration (Millerick-May et al, 2011). Attention should be paid to the removal of cobwebs and maintenance of ventilation. Any external doors to stable blocks and windows within stables should remain open as long as possible to improve ventilation, with a view to reducing respirable particles in the breathing zone of horses (Ivester et al, 2012). This is especially important in areas of high thoroughfare, since human activity produces high concentrations of dust (Samadi et al, 2009), as well as during feeding and cleaning (Woods et al, 1993). It is important to consider the needs of individual patients, as having high thoroughfare or increased ventilation would obviously not be advisable in cases of infectious disease or those in negative energy balance.
The impact of mucking out on dust exposure cannot be understated. During the mucking out process, the concentration of respirable particles within the stable environment increases by up to 20 times above normal range, and up to 10 times in adjacent stables (Clements and Pirie, 2007b). Therefore, if practical, particularly for horses predisposed to severe EAS, stables should be cleaned following removal of horses from the environment (such as for procedures). However, individual horse movements play an even larger role than human activity (Millerick-May et al, 2011; Ivester et al, 2012), so identifying horses that greatly disturb the bedding and create dust clouds in their breathing zone is important. Managing these horses and their surrounding stablemates in a similar manner is advisable. Organic waste, such as urine and faeces, should not be allowed to accumulate because of the increased chance of mould and noxious gas exposure (Hotchkiss, 2019). Bedding should not become a deep litter system, and deep cleaning (including matting) should be performed in between patients, as would be expected for infection control purposes.
Obviously, not all stables can be placed away from the muck heap, roads or hay stores (which should ideally be placed on pallets to reduce moisture build-up) in a hospital environment. However, it is sensible to stable ‘at-risk’ horses away from these areas in order to reduce respirable particle exposure, considering the increased risk of dust exposure associated with these locations (Millerick-May et al, 2011).
Conclusions
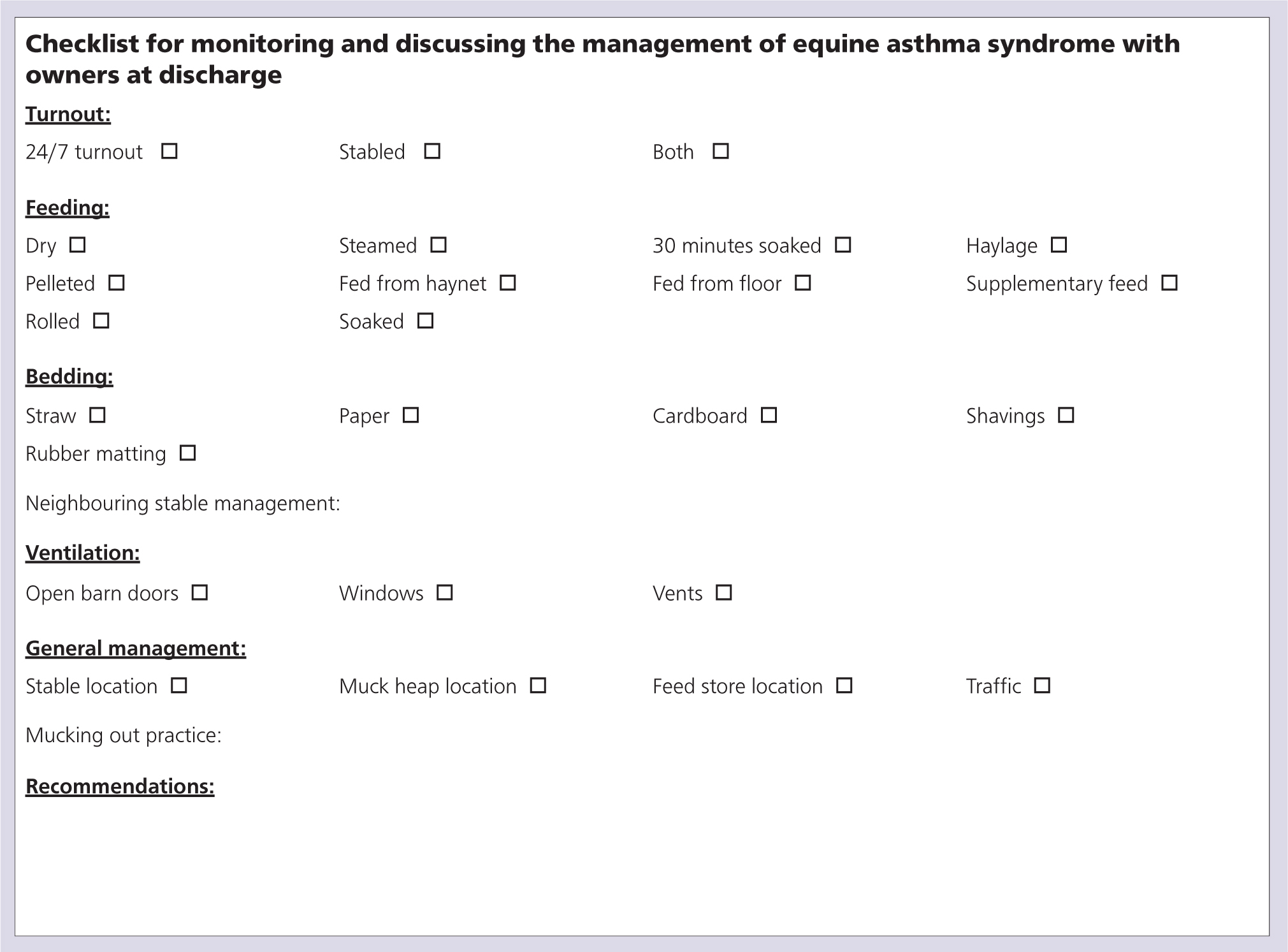
Given how common EAS is within the equine population, it is essential to be aware of appropriate preventative management practices. Ideally these should be applied to all horses within the hospital environment regardless of EAS history. Should signs and physiological changes continue, they can become irreversible and lead to altered respiratory function, airway remodelling, exercise intolerance and even weight loss (Couëtil et al, 2016). In light of the increased risk of morbidity, it is worrying that 50% of owners comply poorly with the recommended management changes given on their yards (Simões et al, 2020). Therefore, taking the time to discuss management changes when discharging patients and use of (or reference to) a checklist is recommended as a means of promoting adherence (Figure 2). While it is acknowledged that not all owners can change their neighbouring stable environment, the importance and impact of it on the breathing zone should be highlighted.
Research into EAS is active and constantly changing, but the importance of minimising dust exposure remains a pivotal factor in the management of these cases. Future directions should therefore focus on identifying thresholds for respirable particle values for the development of EAS, to allow for objective monitoring of the environment. It would also be useful to identify the relative impact of different dust components on the severity of disease exacerbation, as this could allow for more targeted management alterations. Unfortunately, owing to the inability of many owners to alter the whole livery environment, an increased focus on immunological and genetic therapies in the future could aid in reducing inflammation, without relying on the long-term administration of corticosteroids.
KEY POINTS
- Maintaining a dust free environment for all horses is essential, irrespective of whether a horse has been diagnosed with equine asthma syndrome.
- Knowledge of what constitutes a horse's breathing zone is important in understanding what may contribute to the development of clinical signs.
- Horses should be fed from the floor and different dust-reduced forages used, depending on each individual patient's energy balance needs within the hospital environment.
- Management of the stable environment should be performed (if practical) when horses are away for treatments, with ventilation especially important when sweeping barns.
- Knowledge and practice of consultation techniques is essential when providing owners with practical, preventative advice at discharge.


